北京三博脑科医院 - 《三博通讯》
2018-03-28
浏览(73) (0)
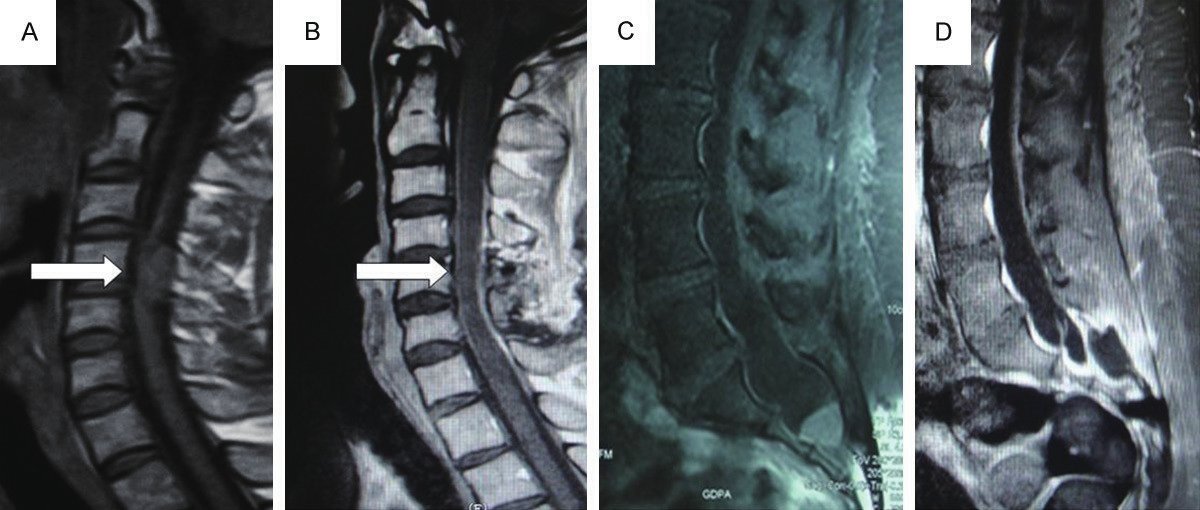
Figure 2. MRI findings of pituitary carcinoma. The First patient: A. MRI shows an intradural extramedullary mass (arrow) at the level of C4-C5, which is isointense on T1WI. B. Postoperative MRI shows no residual tumor (arrow). The second patient: C. MRI shows a homogenously enhancing mass in the sacral canal on T1 post-contrast image. D. Postoperative MRI shows no residual tumor on T1 post-contrast image.
carci- noma (Figure 1D). Postoperative MRI showed that the tumor was totally resected (Figure 2B).
In 2013, he presented with blurred vision. MRI revealed a sellar tumor measuring 1.5 cm in diameter. The patient underwent subfrontal craniotomy for tumor resection on May 23rd in 2013. The morphology of the sellar tumor was similar to that of previous metastatic pituitary carcinoma. There was no recurrence after a 17-month follow-up.
Case 2
A 26-year-old female presented with acromega- ly and amenorrhea 9 years ago. A sellar tumor was noted and removed with a right frontotemporal craniotomy in 2006. The tumor was diagnosed as a pituitary adenoma. In 2012, she developed a recurrent pituitary tumor and presented with acromegaly and amenorrhea. Her serum growth hormone (GH) (121.0 ng/ml) and insulin-like growth factor 1 (IGF-1) (1127.0 ng/ ml) were elevated. Preoperative MRI demonstrated multiple lesions in anterior fossa and sellar region with mild enhancement after gadolinium injection. During the surgery, the tumor was soft and pinkishgrey in color. Since some of tumor tissue tightly adhered to the anterior cerebral artery, subtotal resection was achieved. The histological features are consis- tent with recurrent pituitary adenoma (Figure 1E). Tumor cells
are positive for synaptophysin and growth hormone, but they are negative for other pituitary hormones. The Ki-67 labeling index is approximately 3%. The serum GH (37.8 ng/ml) significantly decreased after operation.
During the hospitalization, she also declared numbness on the left lateral thigh for 6 years. The spine MRI showed a hyperintense well- defined mass in the sacral canal (Figure 2C).Two weeks later, the patient underwent laminectomy at S2-S3 level in order to remove the tumor. During the operation, the tumor was found inside the sacral canal. It was relatively firm in texture and sharply demarcated, and had modest blood supply. At the periphery, the tumor adhered to the bilateral nerve bundles. The histomorphology of the tumor was similar to that of previous surgeries (Figure 1F). The Ki-67 labeling index was 1-2%. Postoperative MRI showed no residual tumor on T1 post-con- trast image (Figure 2D). The serum GH reduced to 29 ng/ml before discharge.
In April 2014, the patient developed a recurrent tumor in the sellar region and was subsequently treated with stereotactic radiation. Recently, the serum growth hormone was 9.5 ng/ml. There was no progression after a 10-month follow-up.